The bane of an injectors practice
In the world of cosmetic enhancements, neurotoxin injections like Botox, Xeomin, Dysport, Jeuveau and now Daxxify have become household names. Revered for their ability to smooth wrinkles and rejuvenate the face, these treatments, however, are not without potential complications. One such complication is eyelid ptosis (pronounced [TOH] + [SIS]) or eyelid droopiness, a condition where the eyelid droops or falls, impacting not only appearance but also, in severe cases, impedes vision.
How Often Does Eyelid Droopiness Occur After Botox?
Drooping Eyelids After Eyelid ptosis or droopiness is a known complication of neurotoxin injections. The incidence rate varies in literature but is generally reported to be between 1% and 5% of patients receiving these treatments. This variance is attributed to factors like injection technique, dosage, and individual patient anatomy. Even highly skilled professionals may see this complication in about 1-2% of their patients, highlighting that it’s not solely a result of poor practice. One study found the occurrence of eyelid ptosis of 5.4% among inexperienced injectors and less than 1% among experienced injectors, focusing primarily on injections in the glabellar and brow area. This means that even a very experienced injector treating 100 patients a month could potentially encounter the complication of eyelid ptosis once per month. Therefore, if an injector claims to have never witnessed this complication in their practice, it may indicate a limited scope of experience, as the occurrence of ptosis is not entirely avoidable, even with the best techniques. This reality underscores the importance of informed consent, where patients are made aware of potential risks, regardless of the injector’s expertise.
How Does Eyelid Ptosis (droopiness) Occur?
The Levator Palpebrae Superioris (LPS): A Key Muscle
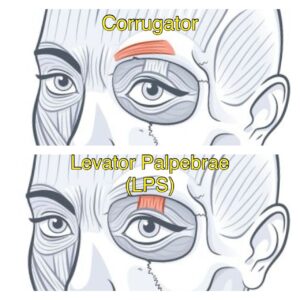
The underlying cause of eyelid ptosis after neurotoxin injection is the unintentional involvement of the Levator Palpebrae Superioris (LPS) muscle, which is responsible for lifting the eyelid. When neurotoxins spread beyond the intended treatment area, they can temporarily paralyze this muscle, leading to eyelid ptosis. It’s important to note that the LPS muscle is not accidentally injected, but the neurotoxin has diffused or spread to the adjacent muscle, the LPS. Eyelid ptosis occurs most commonly with treatment of the glabella aka “angry brow” or “11’s” by injecting the Corrugator and the Procerus. These muscles are in close proximity to the muscle responsible for elevating the eyelid, the LPS. It’s essential to recognize that while improper injection technique may be a factor, eyelid ptosis is a known risk even with experienced injectors.
How Long Will It Last?
The duration of ptosis following neurotoxin injection is typically tied to the longevity of the neurotoxin’s effect. On average, patients may experience ptosis for 3 to 4 weeks. Most cases of ptosis resolve within a month, although it can last up to 3-4 months in rare instances, often due to higher dosing.
How to Prevent Eyelid Droopiness after Botox Injection?
Preventative Measures for Eyelid Ptosis with Neurotoxin Injections
To reduce the likelihood of eyelid ptosis following neurotoxin injections, especially in sensitive areas like the glabella, injectors should employ several key preventative techniques:
- Deep Understanding of Facial Anatomy: Knowing the muscles being targeted, especially the Levator Palpebrae Superioris (LPS), which is crucial for eyelid lifting.
- Careful Placement and Dosage: Injectors should use the minimal effective dose of the neurotoxin and place it precisely to prevent affecting the LPS muscle.
- Refined Injection Techniques: Current techniques for treating the glabella often use a five- or seven-point injection method. Using a 3-point technique can reduce the risk of eyelid and eyebrow ptosis.
- Post-Injection Pressure Application: A practical technique is applying gentle pressure on the area post-injection. After injecting the glabella, the injector can compress the region against the orbit for about 30 seconds. This helps localize the neurotoxin’s effect and reduces its migration.
Patients also play a role in prevention. They should be advised to avoid manipulating the treated area for a certain period after receiving injections, as rubbing or massaging can cause the toxin to spread unintentionally.
By integrating these preventative strategies, including the specific technique of applying pressure post-injection, using minimal effective dosing and using a 3- point injection technique practitioners can significantly diminish the risk of causing eyelid ptosis.
Treatment Options for Eyelid Ptosis
Treatment for neurotoxin-induced ptosis primarily focuses on symptomatic relief until the effect of the neurotoxin wears off. Eye drops like apraclonidine 0.5%, and 0.33% brimonidine topical gel which can provide temporary relief by elevating the eyelid 1-2 mm. Topical brimonidine has been used in dermatology to treat erythematous rosacea because of its potent peripheral vasoconstriction ability.
It’s essential to understand that these medications do not accelerate the resolution of eyelid droopiness. They are merely used for cosmetic purposes until the condition naturally resolves.
Conclusion
While eyelid ptosis is a common complication of neurotoxin injections, its impact on patients’ quality of life and appearance cannot be understated. Understanding the risk factors, muscle anatomy involved, and potential treatments is crucial for both practitioners and patients. As with any cosmetic procedure, a thorough consultation and consideration of individual risks are essential.
1- Kroumpouzos, G., Kassir, M., Gupta, M., Patil, A. and Goldust, M. (2021), Complications of Botulinum toxin A: An update review. J Cosmet Dermatol, 20: 1585-1590.
https://doi.org/10.1111/jocd.14160
2- Yi KH, Lee JH, Hu HW, Kim HJ. Anatomical Proposal for Botulinum Neurotoxin Injection for Glabellar Frown Lines. Toxins (Basel). 2022 Apr 10;14(4):268. doi:
10.3390/toxins14040268. PMID: 35448877; PMCID: PMC9032255.
3- Cotofana S, Pedraza AP, Kaufman J, Avelar LET, Gavril DL, Hernandez CA, Onishi EC, Nikolis A, Sakuma T, Frank K. Respecting upper facial anatomy for treating the
glabella with neuromodulators to avoid medial brow ptosis-A refined 3-point injection technique. J Cosmet Dermatol. 2021 Jun;20(6):1625-1633. doi:
10.1111/jocd.14133. Epub 2021 Apr 16. PMID: 33817912.
4-Scheinfeld, N. (2005). The use of apraclonidine eyedrops to treat ptosis after the administration of botulinum toxin to the upper face. Dermatol Online J, 11(1),
9. PMID: 15748550.
5- Alotaibi,G. F., Alsukait, S. F., Alsalman, H. H., & Turkmani, M. G. (2022). Eyelid ptosis following botulinum toxin injection treated with briminodine 0.33%
topical gel. JAAD Case Rep, 22, 96–98. Published online 2022 Jan 31. doi: 10.1016/j.jdcr.2022.01.019. PMCID: PMC8960886. PMID: 35360374.
Consultation Form
"*" indicates required fields
Consultation Form
"*" indicates required fields


